- Bcs Classification Database Software
- Bcs Classification Database Types
- Bcs Classification Database Training
- Bcs Database Search
- Bcs Classification Tsrl Database
- General Notes On Biopharmaceutics Classification System (BCS ...
Concept paper for comment WHO Drug Information Vol. 1, 2016 4 Pre-publication draft - page numbers are not for citation purposes affect the feasibility of the manufacturing process, including packaging and quality control. The Biopharmaceutical Classification System (BCS) is an experimental model that measures permeability and solubility under prescribed conditions. The original purpose of the system was to aid in the regulation of post-approval changes and generics, providing approvals based solely on in vitro data when appropriate. Importantly, since the majority of drugs are orally dosed, the system was designed around oral drug delivery.
August 26, 2020
Our file number: 20-109235-116
Health Canada is pleased to announce the implementation of International Council for Harmonisation of Technical Requirements of Pharmaceuticals for Human Use (ICH) Guidance M9: Biopharmaceutics Classification System (BCS) Based Biowaivers. This guidance has been developed by the appropriate ICH Expert Working Group and has been subject to consultation by the regulatory parties, in accordance with the ICH Process. The ICH Assembly has endorsed the final draft and recommended its implementation by membership of ICH. In implementing the ICH M9 guideline, it replaces the Health Canada guidance document: Biopharmaceutics Classification System Based Biowaiver. It is recommended that the Health Canada BCS Based Biowaiver Evaluation Template be completed for drug submissions that include a biowaiver request.
As per its commitment to ICH as a standing member, Health Canada is implementing this guidance with no modifications. In implementing this ICH guidance, Health Canada endorses the principles and practices described therein. This document should be read in conjunction with this accompanying notice and with the relevant sections of other applicable Health Canada guidances. This and other Guidance documents are available on the ICH Website. Please note that the ICH website is only available in English. If you would like to request a copy of the French version of the document, please contact the HPFB ICH inbox.
Should you have any questions or comments regarding the content of the guidance, please contact:
Health Canada - ICH Coordinator
E-mail: HPFB_ICH_DGPSA@hc-sc.gc.ca
Dissolution Media
Coning with paddle (USP II)
- PEAK vessel has a cone molded into the bottom using an appropriate tool to eliminate the unstirred cone and the variability concomitant with it.
- Glass cone effectively displaces the unstirred cone, forcing the material tested into the region of appropriate hydrodynamics, where all surfaces of the product are constantly and unifofmJy exposed to the moving medium.
Rapid, Very Rapid Disso. Profiles: Sampling Time Points
Biowaiver and f2 calculation
Alternatives when f2 fails for BCS class 1
FDC Dissolution Profiles
Which Dosage Form?
BCS-based biowaivers are applicable to drug products where the drug substance(s) exhibit
- high solubility and,
- either high permeability (BCS Class I) or low permeability (BCS Class III).
- The BCS-based biowaiver is only applicable to immediate release, solid oral dosage forms or suspensions designed to deliver drug to the systemic circulation.
- Drug products with buccal or sublingual absorption are not eligible for a BCS-based biowaiver application.
- BCS-based biowaiver approach is applicable only when the mode of administration includes water. If administration without water is also intended (e.g., orodispersible products), a bioequivalence study in which the product is dosed without water should be conducted.
- Drug products having a narrow therapeutic index are excluded from consideration for a BCS-based biowaiver
- BCS-based biowaivers are applicable to Fixed-dose combination (FDCs) which are the same dosage form and strength.
- FDC containing only BCS Class Idrugs should meet criteria regarding excipients for a BCS Class I drug.
- only BCS Class III drugs-BCS Class III drugs, Both BCS Class I and BCS Class IIIdrugs, dissolution criteria for the applicable BCS class for each component should be applied.
- BCS Class III drug substances are considered to be more susceptible to the effects of excipients.These drugs are not considered highly permeable and may have site-specific absorption, so there are a greater number of mechanisms through which excipients can affect their absorption than for BCS Class I drugs.
- BCS Class I drugs are highly absorbed, and have neither solubility nor permeability limited absorption. Therefore they generally represent a low risk group of compounds in terms of the potential for excipients to affect absorption, compared to other BCS classes.
- For BCS Class I drugs, qualitative and quantitative differences in excipients are permitted, except for excipients that may affect absorption.
- For BCS Class III drugs, all of the excipients should be qualitatively the same and quantitatively similar (except for film coating or capsule shell excipients).
- For products with more than one strength, the BCS approach should be applied for each strength.
Solubility
Bcs Classification Database Software
A drug substance is classified as “highly soluble” if:
- highest single therapeutic dose or highest strength of the reference product (of dose proportional pharmacokinetics (i.e., AUC and Cmax) )
- completely soluble in 250 ml or lessof aqueous media
- over the pH range of 1.2–6.8 at 37±1°C.At least three pHs including buffers at pH 1.2, 4.5 and 6.8, should be evaluated. In addition, solubility at the pH of lowest solubilityof the drug substance should be evaluated if it is within the specified pH range.
- conducted over a suitable time-frame to reach equilibrium.
- The pH for each test solution should be measuredafter the addition of the drug substance and at the end of the equilibrium solubility study .The pH should be adjusted if necessary.
- Adequate stability of the drug substance in the solubility media should be demonstrated.
- In cases where the drug substance is not stable with >10% degradation over the extent of the solubility assessment, solubility cannot be adequately determined and thus the drug substance cannot be classified.
- Equilibrium solubility experiments may be performed, using a shake-flask technique or an alternative method, if justified.
- For BCS class 1 and 3 compounds, polymorphism is less likely to
impact on bioavailability. - FDA states “For a drug whose absorption is only limited by its dissolution(BCS Class 3 & 4), large differences in the apparent solubilities of the various polymorphic forms are likely to affect BA/BE.
Dose solubility ratio
- Subsequent to the solubility experiments, the dose/solubility ratio (D/S) should be calculated according to the BCS. Whereas a
- D/S > 250 ml in aqueous media indicates solubility issues in the corresponding GI segment(s).
- D/S < 250 ml at all pH values of interest indicates that dissolution is very unlikely to limit drug absorption.
- If the D/S is >250 ml but in the range of 250 to 1,000 ml in all aqueous buffers, solubility experiments should also be performed in biorelevant media.
Permeability
The assessment of permeability should preferentially be based on the extent of absorption derived from
- human pharmacokinetic studies, e.g., absolute bioavailability or mass balance.
- in vitro methods using Caco-2 cells.
High permeability can be concluded when
the absolute bioavailability is ≥85%.
High permeability can also be concluded if ≥85% of the administered dose is recovered in urine as unchanged (parent drug),
or as the sum of parent drug, Phase 1 oxidative and Phase 2 conjugative metabolites.
Regarding metabolites in feces,
- only oxidative and conjugative metabolites can be considered.
- reduction or hydrolysisshould not be included, unless it can be demonstrated that they are not produced prior to absorption, e.g., by microbial action within GIT.
- Unchanged drug in feces cannot be counted toward the extent of absorption, unless appropriate data supports that the amount of parent drug in feces to be accounted for absorbed drug material is from biliary excretion, intestinal secretion or originates from an unstable metabolite (e.g., glucuronide, sulphate, N-oxide)converted back to the parent by action of microbial organisms.
- Changes to adrug product generally have less influence over permeability as this is a property of the drug molecule that is less likely to alter with product and process change.
- Exceptionally, excipients may have an impact on in vivo permeability,either directly on active or passive transit of drug across the gut wall or indirectly by altering the GI transit/residence time.
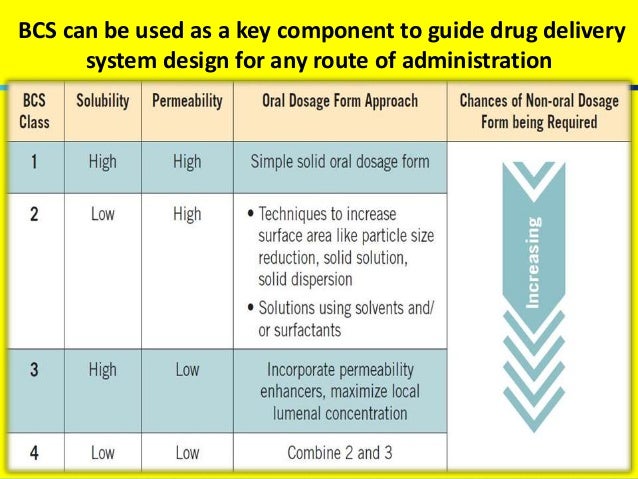
For BCS 2 compounds, a wide range of formulation choices exist.
- Firstly the API should bemicronized to increase
surface area and speed up dissolution. - surfactants or solubilizers should be added to improve wetting and dissolution
- In cases where the compound is ionizable, a pH modifier
(acid or base) may be used to enhance solubility. However,
the use of pH modifiers should be evaluated against in-gut
precipitation due to GI pH gradient. For instance, a basic
compound with pKa around 7 can be solubilized 1,000-fold at
pH 4 with the addition of citric acid. However, the compound dissolved initially in the citric acid vehicle may precipitate out at pH 7 in the lower GI. This phenomenon often accompanies
a truncated absorption phase of short Tmax (less than one
hour post dosing at fasted state). Addition of surfactants
may inhibit nucleation and slow down in-gut precipitation
provided the surfactant travels together with the drug in the
GI track. Combined use of pH modifiers and surfactants
may be more effective in the enhancement of absorption
than pH alone.
For BCS class 3 compounds with high solubility and low permeability,
- Absorption enhancers may be considered for human formulation but
perhaps not for animal formulation. For a dose of 1,000 mg/kg
body weight, a modest 1:2 drug/excipient ratio will require a
dose of the excipient at 2,000 mg/kg body weight. This amount
is often too high for the excipient to be safe without eliciting
excipient-related-toxicity. - API in a capsule, a simple solution or suspensionremains to be the choice toxicological formulations for BCS class 3 compounds.
The introduction of the biopharmaceutics classification system (BCS) in the 1990s made a significant impact on the development of immediate release (IR) oral dosage forms, enabling the use of in vitro data
rather than in vivo human studies for establishing the bioequivalence of low risk (BCS class I) compounds.
Extensions to the biowaiver classes of the BCS have been proposed.
- to class III compounds—provided changes to excipients to enhance solubility doesn’t alter drug permeability,and
- to some class II weak acids on the basis that these drugs often have adequate solubility and permeability in the upper small intestine, so their failure to meet the high solubility criteria at gastric pH has little impact in vivo.
Maximum absorbable dose (MAD)
One of the implications of the MAD equation is that permeability and solubility are compensatory; that is, high permeability may offset low solubilityin determining the maximum dose above which solubility in the GI tract becomes restrictive to absorption.
In one version proposed by Curatolo the derivation uses an absorption rate constant (KA), whilst another by Sun et al. uses an estimate of the
effective human jejunal permeability (Peff).
MAD considers four parameters
- S, solubility at pH6.5 (corresponding to small intestine)
- SIWV, small intestinal water volume (250 mL)
- Tsi, transit time for small intestinea/absorption site (3.32 h or 270 min for the small intestine) and A is the absorption surface area (7.54 X 104 cm2).
- Ka, transintestinal absorption rate
Bioavailable dose is smaller than MAD due to metabolism in portal blood (Liver) and intestinal mucosal tissue.
SLAD (solubility limited absorbable dose)
SLAD considers three parameters:
- Ssi, the small intestine solubility,
- V, the fluid volume (500mL) and
- Mp, the permeability dependent multiplier
SLADconcept, based on the idea that for class II drugs at least, permeability and solubility are compensatory.
The solubility limited absorbable dose(SLAD) is represented
by the boundary between class IIa and IIb for high permeability drugs, and the boundary between class III and IV for low permeability drugs.
Developability Classification System (DCS)
- BCS Class II and IV sub-classification with a, b, and csubclasses dependent on the acidic (a), basic (b), or neutral (c) characteristics of the drug in the physiological pH range (~pH < 7.5).
- The sub-classification, a: for acids (pKa < ~5), b: for bases (pKa > ~5, and c: for neutral drugs (pKa < 0 or ~ >8).
- The WHO BCS Guidance defines that the biowaiver can be extended to BCS Class II weak acids if the API has a “D /S ratio of 250 mL or less at pH 6.8“.
- Solubility criteria stated in present BCS Guidances for classifying an API as “highly soluble” require the highest dosage strength (US FDA) or the highest single dose administered (EMA and WHO) to be soluble at 37°C in 250 mL aqueous buffer solution over :
- pH range of 1.2–6.8according to WHO Guidance (three buffer media pH 1.2, 4.5, and 6.8)
- pH 1.0–6.8 according to EMA Guidance (three recommended buffer media pH 1.2, 4.5, and 6.8), or
- pH 1.0–7.5 according to the US FDA Guidance.
BDDCS (Biopharmaceutics Drug Disposition
Classification System)
- BDDCS could serve as a basis for predicting the importance of transporters in determining drug disposition, as well as in predicting drug–drug interactions.
- The purpose of BDDCS is to predict drug disposition and potential drug–drug interactions in the intestine and the liver with an emphasis on defining which drugs would be amenable to enzymatic-only and transporter-only disposition and drug–drug interactions, as well as where transporter–enzyme interplay may be important.
- In BDDCS, predictions are based on intestinal permeability rate, which was found to be related to extent of drug metabolism. (Whereas, in BCS, biowaivers are based on the extent of intestinal absorption, which in a number of cases does not correlate with intestinal permeability rate.)
- When we exchange the values of R and T –
- Value of difference factor (f1) gets changed.
- Value of similarity factor (f2) remains unchanged.
Similarity factor (f2)
The evaluation of the similarity factor is based on the following conditions:
- A minimum of three time points (zero excluded).
- Not more than one mean value of ≥85% dissolved for either of the products (Onle one measurement should considered after both products have reached 85% dissolution).
- The time points should be the same for the two products.
- Mean of the individual values for every time point for each product.
- To allow the use of mean data, the coefficient of variation should not be more than 20% at early time-points (up to 10 minutes), and should not be more than 10% at other time points.
- An average difference of 10% at all measured time points results in a f2 value of 50.
- FDA has set a public standard of f2 value between 50-100 to indicate similarity between two dissolution profiles.
Bcs Classification Database Types
SUPAC:MR (Scale-Up and Postapproval Changes: Modified Release Solid Oral Dosage Forms) Chemistry,Manufacturing, and Controls; In Vitro Dissolution Testing and In Vivo Bioequivalence Documentation
Bcs Classification Database Training
The guidance defines
(1) levels of change,
(2) recommended chemistry, manufacturing, and controls (CMC) tests for each level of change,
(3) recommended in vitro dissolution tests and/or in vivo bioequivalence tests for each level of change; and
(4) documentation that should support the change.
Bcs Database Search
This guidance specifies application information that should be provided to the Center for Drug Evaluation and Research (CDER) to ensure continuing product quality and performance characteristics of a modified release solid oral dose formulation for specified postapproval changes.
- Components and composition — nonrelease controlling
excipient - Components and composition — release controlling excipient
- Site changes
- Changes in batch size (scale-up/scale-down)
- Manufacturing equipment changes
- Manufacturing process changes
COMPONENTS AND COMPOSITION — RELEASE CONTROLLING
EXCIPIENT
The sponsor should provide appropriate justifications (i.e., mechanism of drug release and manufacturing process) for claiming any excipient(s) as a release controlling excipient in the formulation of the modified release solid oral dosage form.
Level 1 Change-unlikelyto have any detectable impact on formulation quality and performance.(less than or equal to 5% w/w)
Level 2 Change-could have a significant impact. (less than or equal to10% w/w or change in the technical grade and/or specifications)
Bcs Classification Tsrl Database
Level 3 Change-likely to have a significant impact. (greater than 10% w/w or addition or deletion of release controlling excipient)
Thermodynamic, Intrinsic and Kinetic Solubility
- Intrinsic solubility
- equilibrium solubility of the free acid or free base
- fully unionized
- Crystalline phase
- Thermodynamic (or equilibrium) solubility
- as a saturated solution in equilibrium for all species.
- at any pH
- Kinetic solubility
- non-equilibrium solubility (changes with time)
- adding drug’s DMSO solution in aqueous buffer(overestimate solubility)
- Supersaturated solutions (thermodynamically metastable)
- amorphous compound
- fastest dissolving or fastest precipitating species.
REFERENCES
General Notes On Biopharmaceutics Classification System (BCS ...
- https://database.ich.org/sites/default/files/M9_Guideline_Step4_2019_1116.pdf
- https://link.springer.com/article/10.1208/s12248-008-9020-0
- https://www.fda.gov/media/70956/download
- https://pubmed.ncbi.nlm.nih.gov/23147500/
- https://onlinelibrary-wiley com.ezproxy.lib. uh.edu/doi/full/ 10.1002/ jps.23233